What are temporomandibular joint (TMJ) disorders/jaw problems?
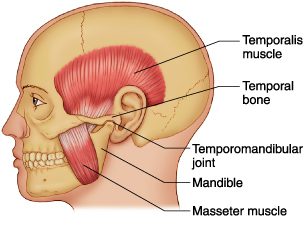
Temporomandibular joint disorders are problems which affect the jaw joint. The jaw joint is located just in front of the ear canal, and it joins the jaw bone (mandible) to the skull near to the temple. The jaw joint is also called the temporomandibular joint (TMJ). Problems affecting this joint are usually known as TMJ disorders or jaw problems. However, there are various other medical terms for for this condition – for example, TMJ dysfunction, TMJ pain and myofascial pain disorder.
Understanding the jaw joint
A joint is where two bones meet. Joints allow movement and flexibility between two bones. The jaw joint allows movement between the jawbone (mandible) and the skull. Muscles attached to the skull and jawbone cause the jawbone to move as the mouth is opened and closed. Inside the jaw joint, there is a smooth material called cartilage, covering part of the bones. There is also a cartilage disc within the joint. The joint is lubricated by fluid called synovial fluid. One could say that the jaw joint resembles the knee joint.
What are the symptoms of temporomandibular joint disorders/ jaw problems?
Temporomandibular joint disorders, more plainly called “jaw problems” are terms describing a variety of signs and symptoms originating from the jaws. These might include pain in the jaws or headaches, reduction of range of jaw movement, jaw stiffness, clicking noises, or dislocation of the lower jaw following certain movements.
The pain is usually located just in front of the ear, and it may spread to the cheek, the ear itself, and to the temple. headaches are very common when the main problem is muscle-related. Jaw movements may be reduced. This may be a general tight feeling or a sensation of the jaw getting stuck. Very rarely, the jaw may get ‘locked’, causing difficulty in opening or closing the mouth. Clicks or noises can sometimes be heard coming from the jaw joint when you chew or move your mouth. These noises can be normal, so they are only relevant if you have other symptoms in the joint, such as pain or reduced movement. Because the ear is very close to the jaw joint, some people get ear symptoms such as noise in the ear, sensitivity to sound or dizziness (vertigo). A most common symptom is headaches and feeling “stiff” jaws, not being able to open the mouth wide; this condition may be associated with muscle spasm and fatigue.
How common are temporomandibular joint disorders?
They are fairly common. About 1 in 10 people have symptoms in the jaw joint at some time in their lives. Of these people, only about 1 in 20 consult a doctor for this problem.
What causes temporomandibular joint disorders?
In general, TMJ disorders are thought to have a ‘multifactorial’ cause, meaning that there are usually a number of factors contributing to the cause. These factors can be grouped into two types: problems linked to the muscles working the joint, and problems inside the joint itself. The muscle problems are the most common type, particularly for younger people.
Problems with the muscles may be caused by:
Over-activity of the jaw muscles. This can occur if you clench your jaw a lot during sleep, which is quite common. Rarely, other conditions make the jaw muscles overactive. Please note that most people who clench their jaws are not aware of this habit. A proper examination will reveal the muscle problems. These muscle pains are perceived as headaches, and most of the times patients have seen a number of doctors and have done several scanning examinations before proper diagnosis.
Increased sensitivity to pain. We don’t know why this happens, but it may be linked to stress, or to some other process which affects pain sensitivity. Some doctors call this type of problem a pain syndrome because the exact cause of the pain is not known.
Problems in the joint may be caused by:
Wear and tear to the inside of the joint – for example, wear and tear to the cartilage. Sometimes this is due to various types of arthritis, the commonest being osteoarthritis or rheumatoid arthritis. This problem tends to affect older rather than younger people. Arthritis means inflammation in a joint.
Injury to the TMJ or to its cartilage disc can cause TMJ pain.
How are temporomandibular joint disorders diagnosed?
Often, the diagnosis is made on the basis of your symptoms and a proper doctor’s examination. In many cases, no tests are necessary if you are healthy and have symptoms that are typical of a TMJ disorder. Possible tests are:
Blood tests which may be helpful to look for signs of inflammation, or to rule out other causes of pain in that area.
An MRI scan which can be used to give a detailed picture of the joint. X-rays are another option, but are used less often now that MRI scans are available.
A diagnostic nerve block which may help to clarify whether the pain is coming from the joint or the muscles. Local anaesthetic is injected near the nerve which goes to the jaw joint. If this relieves the pain, then it suggests that the pain comes from the joint itself.
What is the treatment for temporomandibular joint disorders?

Hard acrylic splint for treatment of TMD
Most problems in the jaw joint can be helped with simple treatments such as painkillers and advice on how to rest the joint, accompanied by some physiotherapy. There are various treatments which are often used in combination:
Resting the jaw joint
You can rest the joint by eating soft food and not using chewing gum. Also, avoid opening the mouth very wide – so don’t do too much singing, and try not to yawn too widely. Massaging the muscles and applying warmth can help.
Other treatments are relaxation and stress-reducing therapies – presumably because people tend to clench their jaw when they are stressed, or because stress makes pain worse.
Splints or bite guards are sometimes suggested. These are made of hard acrylic and are customized to your jaw, usually the upper. They cover the teeth at night to reduce clenching of the jaw. Research shows that they solve muscle issues in a majority of patients.
Medication
Painkillers such as paracetamol, ibuprofen or codeine can help. If these are not enough, muscle relaxants or a small dose of a medicine called a tricyclic antidepressant can give added pain relief.
Physiotherapy
Physiotherapy treatments, such as ultrasound and gentle jaw exercises, can be helpful.
Treatment of other conditions
If there is an underlying condition – for example, a type of arthritis which is contributing to the TMJ disorder – this may need treating in its own right.
What is the outlook for temporomandibular joint disorders?
Generally the outlook is good. Most TMJ disorders improve over time and do not get worse. It is very rare to get any complications with this condition. Some people do have symptoms that last longer or come back (recur), but even these can usually be improved with the treatments described above. Most people do not need injections or surgery and will get better with simple treatments and time.
If you are experiencing headaches or signs of jaw problems/TMD you may arrange for a consultation appointment so we can help you manage the situation together.